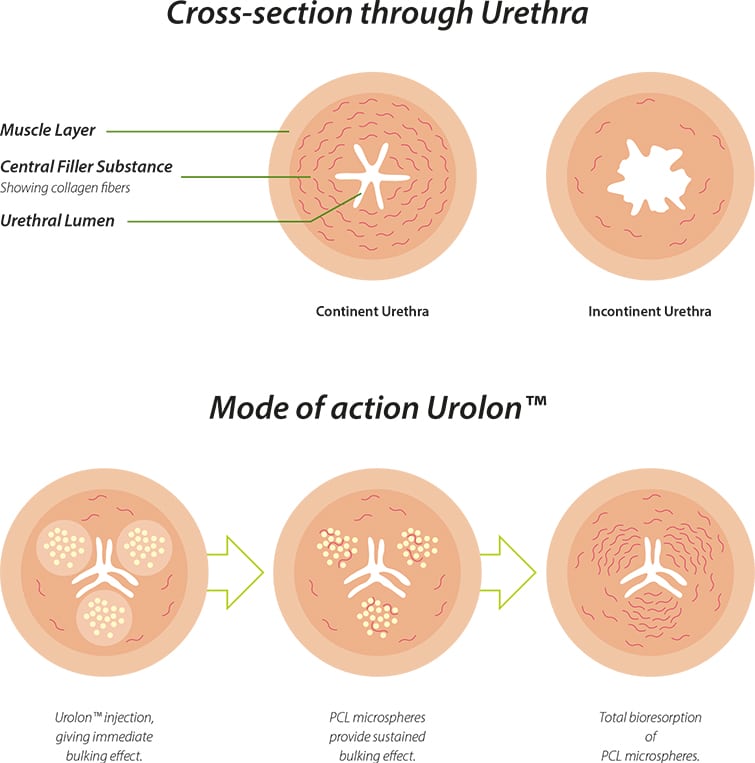
The main constituent of the sub-urethral wall is fibrous connective tissue. Collagen of types I, III, and VI are the predominant component of this connective tissue6. As women with SUI often have a change in their connective tissue metabolism7-9, resulting in altered collagen content, stimulation of collagen production has the potential to replace lost collagen in women with SUI, restoring urinary continence by improving outlet resistance.
Urolon induces a controlled foreign body response and has the potential to induce neocollagenesis in urethral tissue. Studies have shown that an injection of Urolon induces the formation of collagen type I and III. Collagen type III, over several months, is replaced by the more stable collagen type I. This newly formed collagen scaffold embeds the microspheres in the tissue, limiting the risk of dislocation10-11.
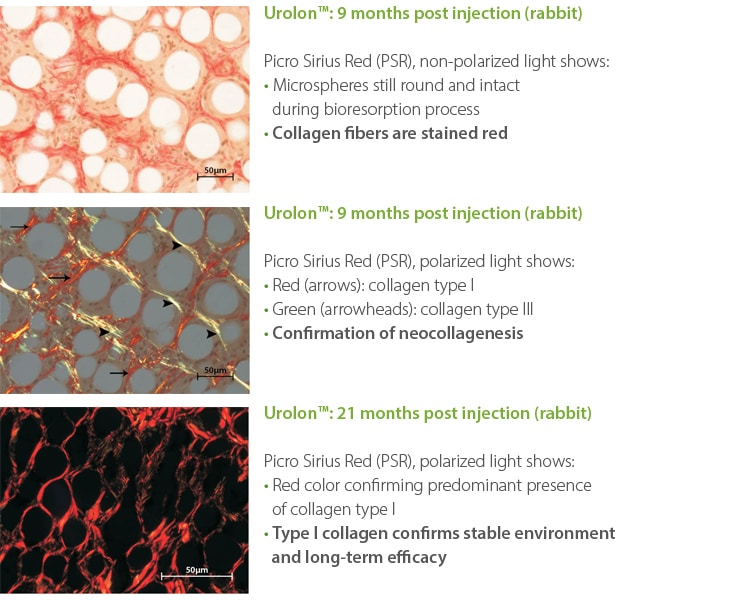
Nicolau PJ, Marijnissen-Hofsté J. Neocollagenesis after injection of a polycaprolactone based dermal filler in a rabbit. Eur J Aesth Med Dermatol, 2013. 3(1): p.19-26
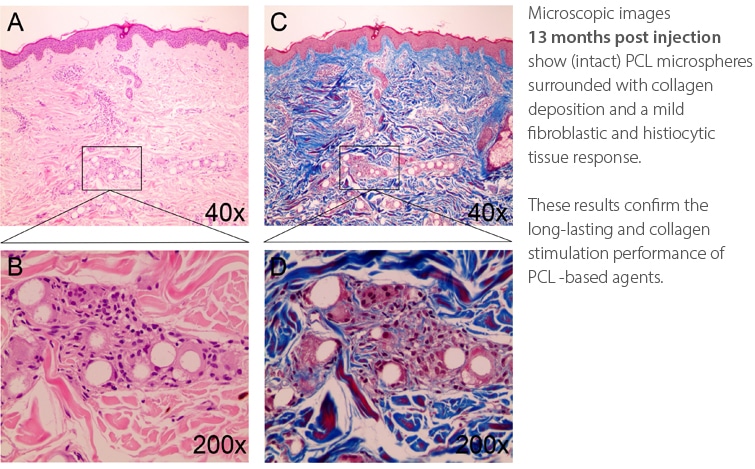
Kim JA, van Abel D. Neocollagenesis in human tissue with a polycaprolactone-based dermal filler. J Cosmet Laser Ther, 2014; early Online: 1-3
Urolon gives an immediate bulking effect primarily from the CMC gel carrier (70%) with subsequent sustained performance due to the highly biocompatible PCL microspheres (30%)10-13. This immediate bulking effect is due to the optimum visco-elasticity of the CMC gel carrier which is key to keeping the PCL microspheres suspended within the gel carrier, and in-situ, once implanted by injection. The CMC gel carrier is gradually resorbed over a period of several weeks to months after treatment.